The Care Quality Commission (CQC) has an important role to play in this age of standards and inspections, which have been established to ensure that all patients receive an appropriate level of care. This briefing covers the way in which the CQC approaches the issue of consent to treatment when carrying out inspections in primary care settings. It emphasises the need to keep sound records of consent conversations between healthcare professionals and patients as evidence of compliance with standards.
The law on consent to treatment
Consent to treatment is an essential part of the modern approach to treating patients with dignity and respect and recognising their autonomy. This is of equal importance in primary, secondary and tertiary care. Informed consent is a legal requirement, by which patients and service users are encouraged to become involved in their care and treatment decisions and must be provided with an appropriate amount of information before they agree to proceed with treatment. Doctors and other healthcare professionals throughout the NHS should receive training and guidance about how to assess the amount of information they should provide to each patient, in view of their individual requirements. Basically, this means that they should be aware that adult service users with capacity should be informed about the diagnosis, the prognosis, and the options for treatment, including the possibility of waiting to see how things develop or simply doing nothing. The risks and benefits of each option should be explained to the service user, and every decision is treatment specific and should be made freely without pressure or undue persuasion of any kind.
It is absolutely essential that the consent conversation with each individual is recorded and kept with the patient’s or service user’s records.
Patients who lack capacity
Healthcare professionals should assume at the outset that all patients have capacity and should not judge a person as lacking capacity simply on the basis of matters such as age or appearance. If a patient has been assessed as lacking sufficient capacity to make a decision about a particular procedure, they should still be involved as far as possible in the decision-making process, and the doctor or other healthcare professional should act in accordance with the patient’s best interests. The Mental Capacity Act 2005 and the Code of Practice made under it give important guidance on this matter, and there is a now large body of case law from which general principles can be drawn about how best to approach this matter, although each patient must be treated as a unique individual. In some instances, there will be a Lasting Power of Attorney in respect of medical decisions which were made before the individual lost capacity, empowering the person to whom the Power of Attorney was granted, to make decisions for the patient in accordance with wishes and in the patient’s best interests. Even if there is no Power of Attorney in place, professionals taking consent are advised to seek information from family members and friends about the patient’s lifestyle, interests, beliefs, cultural and spiritual background when trying to determine what the patient would have wanted and what would be in their best interests. A careful note should be made of the details of the consent process in the case of people who lack capacity.
Children and consent
Primary care and community practitioners should have had training on the law of consent as it concerns children. In the case of very young children, as long as there are no safeguarding concerns, parents should be involved in care and treatment decisions involving their children and should be kept fully informed, bearing in mind the best interests of the children. For older children, the central focus is the Gillick case in which the highest UK Court ruled that children under 16 who have been assessed as competent to consent for themselves, should be informed about their clinical condition and treatment options in the same way as adults with capacity. The case law indicates that the more complex the treatment, the greater the capacity required for the child to give consent. The courts have also given careful consideration to the best way for healthcare professionals to approach the question of maintaining the medical confidentiality of the child, and it is accepted that parents’ right to be kept fully informed about their children’s treatment is “dwindling in nature” as the child grows closer to the age of 16. In many instances, the confidentiality of older children must be protected even if parents ask healthcare professionals to divulge details. Obviously, each child must be treated as a unique individual and in some very complex situations, often involving termination of pregnancy or contraceptive advice, courts have been asked for guidance. Again, it is essential to keep detailed records of consent conversations and to record the reasons for taking the approach that was chosen by the healthcare professional.
The approach of the CQC when regulating consent to treatment
CQC Regulation 11 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 deals with consent to treatment, and this important Regulation was introduced to ensure that all service users, including patients and people acting on their behalf, have given consent in advance of receiving treatment. The CQC inspectors investigate whether consent has been obtained lawfully by providers and whether the person taking consent has the required knowledge and understanding of the care and/or treatment in question. The CQC must refuse registration if providers are unable to satisfy them that they are able and willing to comply with this regulation.
While the CQC treats consent as an important aspect of providing care and treatment, in some cases, acting strictly in accordance with consent will mean that some of the other regulations cannot be met. Providers must never provide unsafe or inappropriate care simply because the patient has consented to care or treatment that would be unsafe.
The CQC can prosecute an organisation for a breach of the Regulation or part of it and can directly initiate a prosecution without first serving a Warning Notice. The CQC may also take other regulatory action.
An example of a Trust fined by the CQC for breaching Regulation 11
Although this example involves an NHS Trust, all health and social care providers should take note of what happened when there was a breach of the consent Regulation because the same standards need to be met wherever the patient is treated.
Two fixed penalty notices were issues and a fine totalling £8,000 was imposed on the Trust in this case by the CQC for breaching the regulatory requirements concerning consent and compliance with the Mental Capacity Act 2005.
The facts of the case
The case concerned a patient who was believed by Trust staff to lack capacity to make decisions about his care and treatment. The CQC found on inspection, that assumptions had been made about the patient’s lack of capacity and concluded that staff should have done more to communicate with him in a way that he was able to understand. The CQC took swift criminal enforcement action against the Trust.
The patient, aged 55, had been deaf since birth and had been diagnosed with epilepsy and autism. He had undergone medical procedures in hospital which involved feeding tubes required for nutritional support. The Trust staff had decided that the patient lacked capacity to consent to the procedures. However, the CQC found that it had done so without carrying out a proper assessment of the patient’s mental capacity, and without making enough effort to communicate with him at every point in a way that he understood.
The staff had made the following mistakes:
- not attempting to arrange for a British Sign Language interpreter to be involved in communicating with the patient
- not involving family members,
- failing to consult appropriately with the holder of the patient’s Lasting Power of Attorney (contact had been made with the Attorney in relation to only one of the procedures),
- not keeping a record of how the best interests decision was made,
- not documenting the capacity assessments
Although the CQC was satisfied that Trust-wide training and policies concerning consent and mental capacity were in place, there were issues of concern in connection with oversight, monitoring, audit and completion of training, where the emphasis should have been on ensuring that policies and training were actually followed in practice.
This case reveals that there is a high level of scrutiny by the CQC in consent matters, and especially in respect of care and treatment of people with autism and learning disabilities, as part of its focus on inequalities in healthcare.
Taking consent under different working conditions in primary care.
During March 2020, the CQC noted that general practice had begun to move to new ways of working, including the use of ‘total triage’ and online or remote consultations . Data from NHSX indicates that by 1 June 2020, 87% of general practices had gone live with technology to enable online consultations, and that figure has increased markedly during the COVID-19 period. The main concern of the CQC was that systems used by GP practices had not fully reflected these rapid shifts in ways of working. Methods of recording GP activity are still at the “experimental” stage, and data generally only covers appointments delivered in traditional ways, but it became clear that during lockdowns there were far fewer face to face consultations and an increased proportion of telephone consultations.
Conclusion
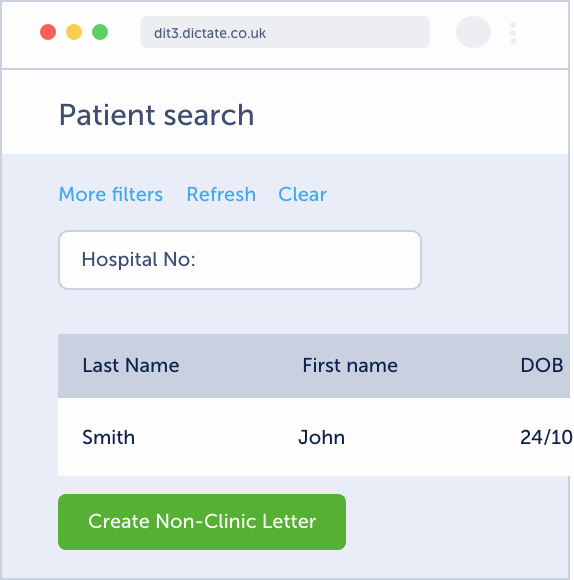
It is important for senior GPs and practice managers to ensure that all staff working in primary care settings are adequately trained on all aspects of consent to treatment. As primary care practitioners are under more pressure than ever, it is important not to ignore the need to update training on consent, taking account of new ways of having consent conversations, carrying out capacity assessments, and importantly, keeping detailed and accurate records of training courses attended by staff. Details of consent conversations and of decisions made by patients should be recorded and kept with the patient’s notes. During any inspection by a Regulator, it is vital to be able to produce evidence that the correct procedures on consent have been followed. The best evidence is contemporaneous written evidence and all documents containing details demonstrating that standards have been met should be stored electronically and should be accessible with ease.
[i] Regulation 11 states:
- Care and treatment of service users must only be provided with the consent of the relevant person.
Paragraph (1) is subject to paragraphs (3) and (4). - If the service user is 16 or over and is unable to give such consent because they lack capacity to do so, the registered person must act in accordance with the 2005 Act*.
- But if Part 4 or 4A of the 1983 Act** applies to a service user, the registered person must act in accordance with the provisions of that Act.
- Nothing in this regulation affects the operation of section 5 of the 2005 Act*, as read with section 6 of that Act (acts in connection with care or treatment).
* Mental Capacity Act 2005
** Mental Health Act 1983”
[ii] The CQC report on the lockdown practices stated that of 1.34m appointments on Monday 2 March 2020, 15% were recorded as being by phone; and on Monday 30 March 2020, a week after the start of the first lockdown, there were 0.93m appointments, of which 46% were recorded as being by phone. In April, the number of appointments delivered via traditional modes, including the proportion of face-to-face appointments, had started to rise again. However, during the same period, were more than a million extra calls were made to NHS 111 in England, in response to the public campaign to highlight the need to contact 111 first with any concerns. The number of calls almost doubled in March 202 in comparison with preceding months but fell back to more normal levels in April.
This article was written for Dictate.IT by Professor Vivienne Harpwood.